Abstract

Introduction : Inotuzumab ozogamicin (InO) is an antibody-drug conjugate approved in the US and the European Union for relapsed/refractory acute lymphoblastic leukemia (R/R ALL). The approved starting dose is 1.8 mg/m 2/cycle in 3 divided doses. Patients receiving this dose of InO in the phase 3 INO-VATE trial had a higher rate of remission and were more likely to proceed to hematopoietic cell transplantation (HCT) than those in the chemotherapy arm. However, compared with patients who received chemotherapy, patients who received InO were more likely to experience post-HCT hepatic sinusoidal obstruction syndrome (SOS, previously called veno-occlusive disease or VOD). It is not known whether a lower dose of InO would improve safety and reduce the likelihood of post-HCT SOS and whether this would impact efficacy. This phase 4 study (NCT03677596) is a post-marketing requirement of the US Food and Drug Administration, and aims to evaluate the efficacy and safety of two dose levels of InO in adults with R/R ALL who are eligible for HCT and who have a higher risk of post-HCT SOS.
Methods : This ongoing, open-label phase 4 study will involve approximately 102 patients with R/R ALL who are eligible for HCT and who have a higher risk of post-HCT SOS. The run-in phase was the first phase of this study, and followed a Simon two-stage design, where 22 patients (7 in stage 1 and 15 in stage 2) received a starting dose of 1.2 mg/m 2/cycle in 3 divided doses. To proceed to the randomized phase, this dose of InO needs to show acceptable efficacy in the run-in phase, meaning the rate of complete remission (CR)/CR with incomplete hematologic recovery (CRi) needs to be ≥3/7 in stage 1 and ≥10/22 by the end of stage 2, with minimal residual disease (MRD) negativity ≥7/22. In the randomized phase, approximately 80 patients will be randomized to receive InO either at the lower starting dose (1.2 mg/m 2/cycle) or the currently approved dose (1.8 mg/m 2/cycle). Patients are being followed for overall survival, disease status, subsequent treatments and adverse events (AEs) for ≥2 years following randomization. This interim analysis reports the efficacy and safety of InO at the lower dose level, based on data from the run-in phase of this study, up to July 30 th 2020.
Results: In the run-in phase of this study, 22 patients received InO at the lower starting dose (1.2 mg/m 2/cycle), for a median duration of 6 (range 0.1-22.7) weeks, and a median of 2 (range 1-6) treatment cycles. Median age was 46 years (range 21-67), and 54.5% patients were male. At baseline, risk factors for post-HCT SOS included previous HCT (31.8%), salvage ≥2 (68.2%), age ≥55 (22.7%), and prior or ongoing hepatic disease (27.3%). Half of patients discontinued treatment (11/22). Reasons for discontinuation were death (n=3), progressive disease (n=7) and relapse (n=1).
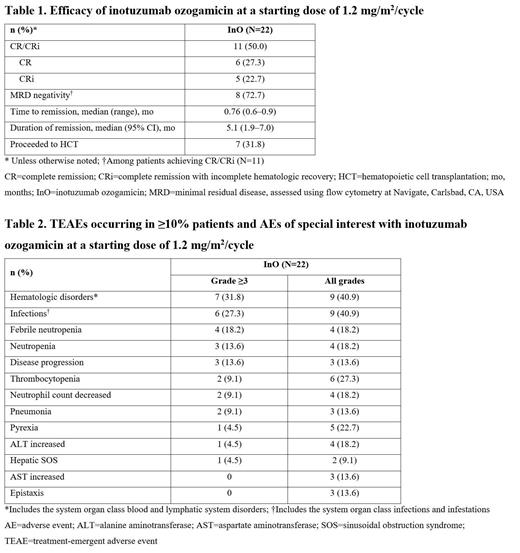
In stage 1 of the run-in phase, 3/7 patients achieved CR/CRi (CR: 2, CRi: 1), and the trial proceeded to stage 2. By the end of stage 2, half of patients achieved CR/CRi, with over 70% of these patients being MRD negative (Table 1). Almost a third of patients proceeded to HCT (31.8%). Three patients died during treatment and 10 died after treatment (4 in disease follow-up and 6 in long-term follow-up). Causes of death were disease progression (n=7), AEs not related to study treatment (n=4), hepatic SOS (n=1), and sepsis (n=1).
Treatment-emergent AEs (TEAEs, any grade) occurred in 90.9% (20/22) patients, and 59.1% (13/22) had a treatment-related AE. The most common grade ≥3 TEAEs included hematologic disorders and infections (Table 2). Of patients who proceeded to HCT, 28.5% (2/7) had post-HCT SOS: one was grade 5 (a patient with ongoing or prior hepatic disease) and the other was grade 2 (a patient in salvage ≥2 with prior HCT). There were an additional five grade 5 AEs: disease progression (n=3), and infections (n=2). Two patients (9.1%) discontinued due to AEs (tumor lysis syndrome and fungal infection). Three AEs led to dose interruption for two (9.1%) patients (catheter-related infection, pyrexia and megaloblastic anemia). There were no dose reductions due to AEs.
Conclusions: At a starting dose of 1.2 mg/m 2/cycle, InO showed acceptable efficacy, with half of patients achieving remission, and more than 70% of those in remission being MRD negative. No new safety signals were identified, and two patients had post-HCT SOS. This phase 4 study is therefore proceeding to the randomized phase, with 69 patients randomized as of July 2021.
Özcan: Pfizer: Research Funding; Bayer: Research Funding; MSD: Research Funding; BMS: Other: Travel/Accommodations/Expenses; Janssen: Other: Travel/Accommodations/Expenses, Research Funding; Archigen: Research Funding; Celgene: Research Funding; Abbvie: Other: Travel/Accommodations/Expenses, Research Funding; Amgen: Honoraria, Other: Travel/Accommodations/Expenses; Takeda: Honoraria, Other: Travel/Accommodations/Expenses, Research Funding; Jazz: Other: Travel/Accommodations/Expenses; AstraZeneca: Research Funding; Abdi Ibrahim: Other: Travel/Accommodations/Expenses; Roche: Other: Travel/Accommodations/Expenses, Research Funding; Sanofi: Other: Travel/Accommodations/Expenses. Cassaday: Vanda Pharmaceuticals: Research Funding; Amgen: Consultancy, Research Funding; Merck: Research Funding; Pfizer: Consultancy, Research Funding; Kite/Gilead: Consultancy, Honoraria, Research Funding; Pepromene Bio: Membership on an entity's Board of Directors or advisory committees; Servier: Research Funding. Zhang: Pfizer: Current Employment, Current equity holder in publicly-traded company. Nègre: Pfizer: Current Employment, Current equity holder in publicly-traded company. Vandendries: Pfizer: Current Employment, Current equity holder in publicly-traded company.
Inotuzumab ozogamicin (InO) is approved in the US for relapsed/refractory acute lymphoblastic leukemia (R/R ALL) at a starting dose of 1.8 mg/m2/cycle in 3 divided doses. This publication reports on the use of InO for R/R ALL at a starting dose of 1.2 mg/m2/cycle in 3 divided doses.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal